New study with UCLA researchers finds improvements to T-cell therapy for cancer

By Aditi Kumar
Aug. 28, 2022 10:26 p.m.
Researchers from UCLA, Stanford University and the University of Pennsylvania have created a system that could improve upon an existing type of therapy for cancer known as T-cell therapy.
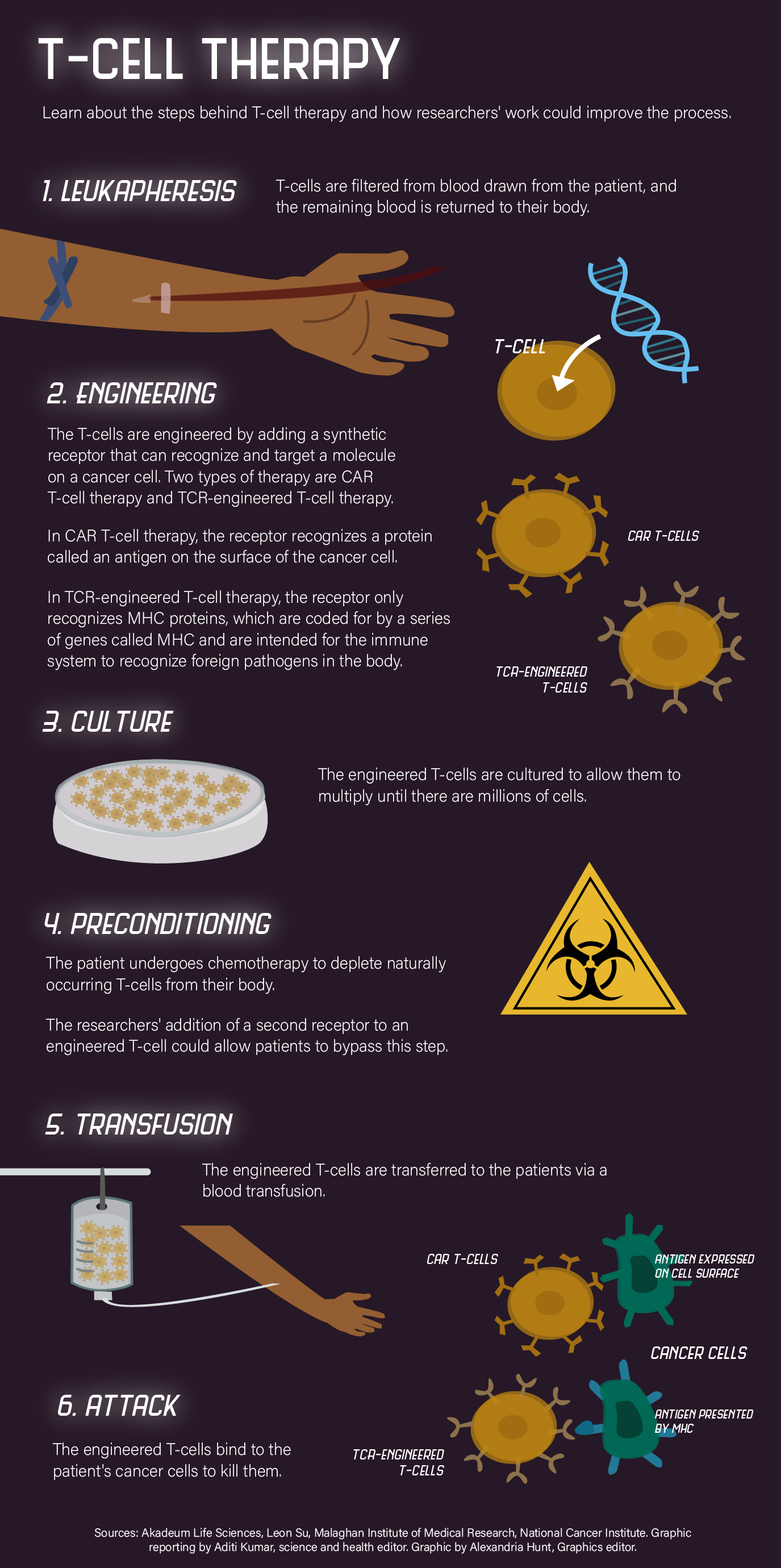
T-cells, a type of immune cell in the body, can mount a response against cancer cells, although their response is not strong enough, said Dr. Anusha Kalbasi, an assistant professor of radiation oncology at the David Geffen School of Medicine. He added that T-cell therapy research focuses on engineering T-cells to allow them to target cancer cells with greater precision. Kalbasi said these therapeutic T-cells need to compete with naturally occurring T-cells to multiply in the body.
Patients undergo chemotherapy to decrease the number of naturally occurring T-cells in the body, a process called preconditioning, said Leon Su, a staff research scientist in the Garcia Lab at Stanford University, adding that preconditioning can cause many negative side effects for patients.
In a study published June 8, the researchers described how they engineered T-cells to include an additional receptor, allowing them to respond to a signal created by the researchers that directs the cells to grow.
Su, a co-author of the study, said that in engineering the therapeutic T-cells with this receptor, the researchers tested them on cancer tumors in mice and on human cancer cells cultured in a lab.
Two types of existing T-cell therapy were engineered with the receptor: CAR T-cell therapy and TCR-engineered T-cell therapy, said Kalbasi, who is also a co-author of the study. He added that the CAR T-cell therapy version was tested on human and mouse models of melanoma and the TCR-engineered therapy version on human and mouse models of pancreatic cancer.
Mikko Siurala, co-founder and head of oncolytics at Dispatch Biotherapeutics – a cancer therapy start-up company – said the pancreatic cancer model was created at the University of Pennsylvania. After administering the therapy, they saw a complete response, meaning they were able to kill the tumor, and it did not relapse.
Kalbasi said similar results were seen in the melanoma model used at UCLA.
Su said the signal for cell growth is a mutated version of a type of molecule called a cytokine that is naturally occurring in the body.
Only therapeutic T-cells will proliferate when the engineered cytokine is administered by the researchers, eliminating the need for patients to undergo preconditioning prior to receiving T-cell therapy, said Kalbasi.
“Anytime you can reduce the number of perturbations a patient has to undergo before they even get their therapy is beneficial to them,” Su said.
Kalbasi added that the new receptor is chimeric, meaning its extracellular domain, the portion outside of the cell, and the intracellular domain, the portion inside the cell, are not from the same receptor.
Su said the intracellular domain is from the IL-9 receptor that results in an IL-9 signal being generated within the cell, which is associated with growth and longevity.
“You kind of want a cell that can proliferate but also has the effector function, and you want a cell that can be engrafted and persist over time,” Su said. “That’s kind of the holy grail of T-cell immunotherapy.”
Treating solid tumors – those consisting of a mass of tissue as opposed to blood cancers – comes with unique challenges, Kalbasi said. T-cells need to travel from the blood into the tissue to reach the tumor, which creates an environment that suppresses the immune system and is hostile to T-cells, he added.
Kalbasi said their engineered receptor-cytokine system attempts to overcome both of these challenges, as the IL-9 signal improves both the T-cell’s ability to reach the tumor and to resist the hostile environment.
In the future, Kalbasi and Su said they hope to continue to improve their therapy. Su said he wants to continue to study the mechanism behind the IL-9 signal and engineer the intracellular domain of the receptor to increase the signal’s strength and improve the T-cell’s ability to persist. Kalbasi said he wants to study the therapy to see if it could cause an immune response in patients.
Siurala, a co-author of the study and former postdoctoral scholar at the University of Pennsylvania, said Dispatch Biotherapeutics is working toward the goal of bringing this system to clinical trials.
“There are many cases in history where people have seen this kind of responses in mice, and they’re very optimistic, and then something goes wrong, and then the therapy doesn’t work in us (humans),” Siurala said. “But I remain optimistic about the impact of this in cancer patients.”