UCLA-developed i-insulin could mitigate risk of hypoglycemia for diabetes patients
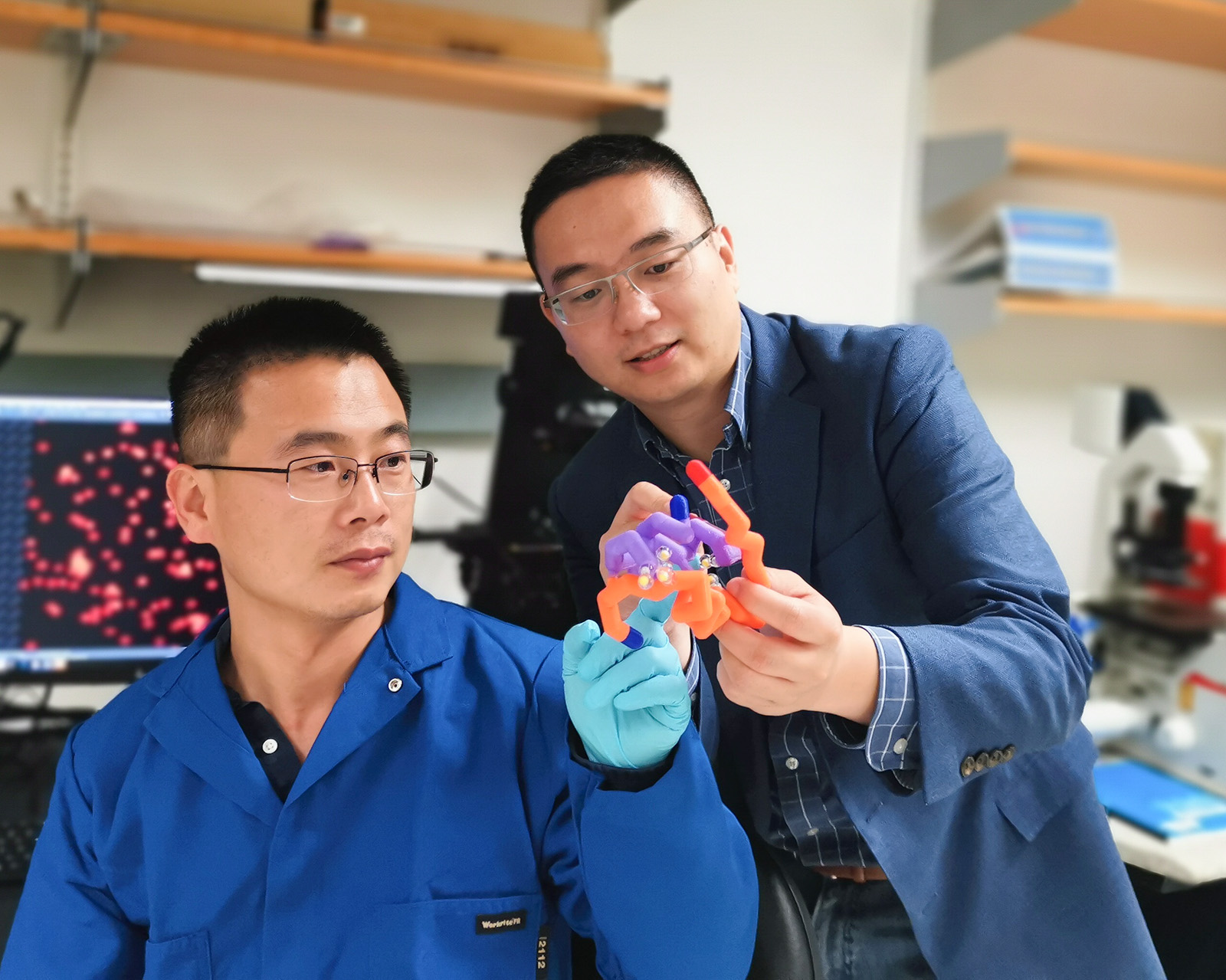
Jinqiang Wang, a postdoctoral researcher, and Zhen Gu, a UCLA bioengineering professor, have helped develop a new type of insulin that could prevent low blood sugar in patients with diabetes. (Courtesy of UCLA Newsroom)

By Sameera Pant
June 6, 2019 12:48 a.m.
A UCLA-led research team has developed a new type of insulin that could prevent low blood sugar in patients with diabetes.
Zhen Gu, the study’s principal investigator and a UCLA bioengineering professor, helped develop a new type of insulin, called i-insulin, that automatically responds to changes in blood glucose levels. This could potentially help patients with diabetes regulate their blood sugar.
Conventional forms of insulin treatments require diabetic patients to repeatedly self-administer insulin injections and keep track of their blood glucose levels themselves. I-insulin, on the other hand, is self-regulating, which can lower the risk of human error.
Insulin, a hormone produced by the pancreas, regulates the level of sugar present within the blood. Diabetes, a disease that affects more than 400 million people across the world, is characterized by high blood sugar levels.
Insulin can be described as a “key” that fits a particular part of a cell and the insulin receptor a “lock,” said John Buse, study co-author and director of the Diabetes Care Center at the University of North Carolina at Chapel Hill School of Medicine.
“(Insulin) opens the doors, through which sugar molecules enter cells for storage and processing,” Buse said. “So in muscle cells and fat cells, where we store energy to be able to generate heat when it’s cold and move around, … sugar only enters those cells in the presence of insulin.”
Diabetes exists in two forms: Type 1 and Type 2. Type 1 diabetes is caused by the destruction of insulin-producing cells, while Type 2 is caused by the inefficiency of insulin produced in the body, Buse said.
I-insulin takes advantage of glucose transporter molecules, the proteins that enable the transportation of glucose in and out of cells. These molecules are tailored to carry insulin throughout the body, Gu said in an email statement.
The i-insulin becomes active when blood sugar levels are high. Conversely, when the blood sugar is dangerously low, the insulin remains inactive, Buse said.
Insulin therapy can lead to hypoglycemia or low blood sugar, Buse said.
“If you give too much insulin, the blood sugar can get too low,” Buse said, “It can actually get so low that people pass out, have seizures, go into a coma or even die.”
I-insulin reduces the risk of hypoglycemia by sensing blood glucose levels and changing its activity accordingly, said Jinqiang Wang, the study’s co-lead author and a postdoctoral researcher in Gu’s research group, in an email statement.
Researchers have successfully completed animal testing for i-insulin and plan to conduct clinical trials soon. If i-insulin is approved for clinical use, patients with diabetes might need to take only one shot of i-insulin a day, Buse said.
Buse said i-insulin could eventually be administered through a skin patch rather than an injection.
Although i-insulin would primarily be used to treat Type 1 diabetes, it could potentially help treat Type 2 diabetes as well, Buse said.
Gu said he and his team are still working on making i-insulin even more responsive to changes in blood glucose levels.
Buse added that more detailed testing of how safe i-insulin is for humans would also be necessary.
“(We need) to do some more detailed testing around human safety,” Buse said “There’s a variety (of tests) we can use to determine whether something has a cancer risk or whether it has a (genetic) risk.”
Gu said his lab is focusing on improving i-insulin delivery methods to administer the treatment more easily, reduce the pain of the treatment and improve its efficacy.
“We do hope our technology could help people with diabetes,” Gu said.
Buse said he thinks the research is well-positioned to move forward and holds potential for improving diabetes treatment.
“Of the smart insulin projects I’ve worked on with (Gu), I think this has the greatest promise to really solve the problem of diabetes care,” Buse said.