Recent NIH grant funds UCLA HIV research with aims to find a cure through inactive cells
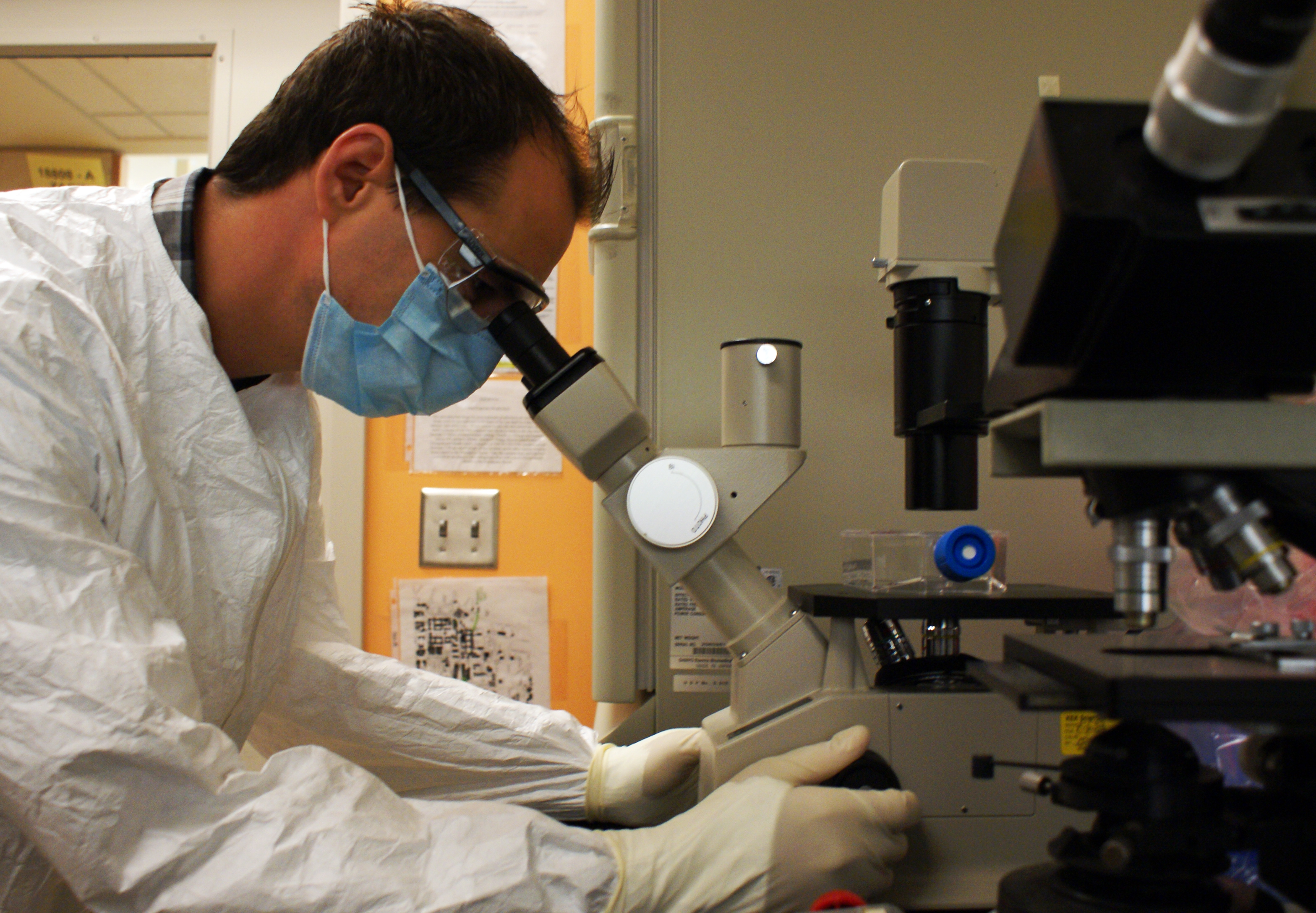
UCLA AIDS Institute researcher Matthew Marsden is helping to work for a cure against HIV at the Biomedical Sciences Research Building.
By Lynn Rice
Aug. 1, 2011 1:33 a.m.

UCLA researcher Matthew Marsden’s work on the eradication of HIV/AIDS is being partially funded by a recent donation from the National Institutes of Health. The grant is part of a larger project with teams across the country.
Matthew Marsden stands in front of a fume hood that pumps a layer of protective air between himself and his experiments and continuously draws the air inside through HEPA filters, self-sanitizing with UV light between experiments.
He suits up in a water-repellent, disposable lab coat, goggles, double gloves and a face mask.
Marsden, a researcher with the UCLA AIDS institute, conducts experiments on HIV in his laboratory in the Biomedical Sciences Research Building. He is part of a group working to develop medication that, in a limited number of treatments, could completely rid infected individuals of HIV.
An HIV diagnosis today means imbibing daily drug cocktails with price tags that can exceed $1,000 a month. But although these medications must be taken every day, the drugs do not eliminate HIV. They only keep it at bay.
Marsden’s research team, however, is setting out to change this. The team uses mice that cost $150 each with immune systems implanted with human tissue, modified to resemble the immune systems of human beings.
They use the mice to see how humans will react to medications that attempt to eliminate HIV from the body.
Using mouse models to study HIV was thought to be impossible until the team proved otherwise, said Jerome Zack, director of the UCLA Center for Aids Research and UCLA professor in the departments of microbiology, immunology and molecular genetics and medicine. The mice are a low-impact alternative to the human and primate models traditionally used in the field, he added.
The team’s efforts have most recently gained the backing of the National Institute of Allergy and Infectious Diseases, a division of the National Institutes of Health.
The leader of the NIAID initiative, David Margolis of the University of North Carolina at Chapel Hill, said Zack was among the first researchers in the country to describe HIV latency and persistence.
He added that the mouse model by Zack’s team expands the repertoire of testing available, which will also include primate models and, eventually, humans.
“A lot of this collaboration is focused on drug-based models,” said Margolis, a professor of medicine, microbology and immunology, and epidemiology. “(Zack’s) approach brings human immunology into the picture.”
The NIAID is donating $14.6 million to HIV research teams across the country, which includes $250,000 to a team headed by Zack. The grant funds the nation’s leading experts in a collaborative effort to draw out and destroy the cells that have rendered HIV so evasive.
Zack’s lab is working with 15 teams, including UNC, in four core academic facilities across the country to draw out and destroy latent HIV-infected cells.
Some cells infected with HIV will replicate. Such cells are easily destroyed by current anti-HIV medication. However, other infected cells lie dormant in the body.
Those cells, which do not respond to medication, are the targets of the grants.
“As soon as you know you have HIV, you already have one million latent cells in your body that you can’t do anything about,” Zack said.
Inactive HIV-infected cells aren’t eliminated by current treatments. These cells are not detected during HIV screenings and can be activated at any time, especially if medication is interrupted or if patients develop a resistance to medication, Zack said.
This is a deadly combination for patients. Such infected cells can sit latent for decades before replicating, compromising the body’s immune system, Zack said.
With successful results, groups researching HIV-eradication strategies may be eligible to renew funding for up to five years, according to email statements from NIAID representatives.
The goal being pursued is unprecedented, Zack said. Even three years ago, leading researchers and scientists did not consider the eradication of HIV in the body to be possible.
But for now, the timeline of a cure is still indefinite.
“We’d love to say that we could cure HIV by the end of this grant’s five years,” Zack said. “But in this field, we’ve learned better than to make predictions.”